Research shows that use of tobacco, alcohol, or illicit drugs or abuse of prescription drugs by pregnant women can have severe health consequences for infants. This is because many substances pass easily through the placenta, so substances that a pregnant woman takes also, to some degree, reach the baby.
Recent research shows that smoking tobacco or marijuana, taking prescription pain relievers, or using illegal drugs during pregnancy is associated with double or even triple the risk of stillbirth.
Risks of Stillbirth from Substance Use in Pregnancy
- Tobacco use—1.8 to 2.8 times greater risk of stillbirth, with the highest risk found among the heaviest smokers
- Marijuana use—2.3 times greater risk of stillbirth
- Evidence of any stimulant, marijuana, or prescription pain reliever use—2.2 times greater risk of stillbirth
- Passive exposure to tobacco—2.1 times greater risk of stillbirth
Regular drug use can produce dependence in the newborn, and the baby may go through withdrawal upon birth. Most research in this area has focused on the effects of opioid misuse (prescription pain relievers or heroin). However, more recent data has shown that use of alcohol, barbiturates, benzodiazepines, and caffeine during pregnancy may also cause the infant to show withdrawal symptoms at birth (Hudak et al., 2012). The type and severity of an infant’s withdrawal symptoms depend on the drug(s) used, how long and how often the birth mother used, how her body breaks the drug down, and whether the infant was born full term or prematurely (Neonatal abstinence syndrome, 2014).
Symptoms of drug withdrawal in a newborn can develop immediately or up to 14 days after birth and can include:
- blotchy skin coloring
- diarrhea
- excessive or high-pitched crying
- abnormal sucking reflex
- fever
- hyperactive reflexes
- increased muscle tone
- irritability
- poor feeding
- rapid breathing
- increased heart rate
- seizures
- sleep problems
- slow weight gain
- stuffy nose and sneezing
- sweating
- trembling
- vomiting
Effects of using some drugs could be long-term and possibly fatal to the baby:
- low birth weight
- birth defects
- small head circumference
- premature birth
- sudden infant death syndrome (SIDS)
Illegal Drugs
Also See : Marijuana Addiction
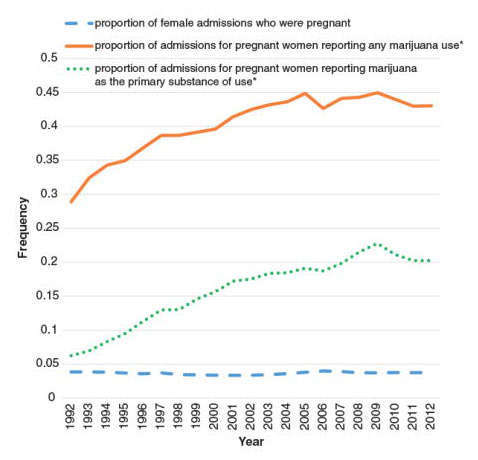
More research needs to be done on how marijuana use during pregnancy could impact the health and development of infants, given changing policies about access to marijuana, as well as significant increases over the last decade in the number of pregnant women seeking substance use disorder treatment for marijuana use (Martin et al., 2015).
There is no human research connecting marijuana use to the chance of miscarriage (Kline et al., 1991; Wilcox et al., 1990), although animal studies indicate that the risk for miscarriage increases if marijuana is used early in pregnancy(Asch & Smith, 1986). Some associations have been found between marijuana use during pregnancy and future developmental and hyperactivity disorders in children(Campolongo et al., 2011; Fried et al., 1992; Goldschmidt et al., 2000; Fried & Smith, 2001). Evidence is mixed as to whether marijuana use by pregnant women is associated with low birth rate (Janisse et al., 2014; Hayatbakhsh et al., 2012; Shiono et al., 1995; Mark et al., 2015; Schempf & Strobino, 2008) or premature birth (Mark et al., 2015), although long-term use may elevate these risks (Shiono et al., 1995). Pregnant women are strongly discouraged from using marijuana, given its potential to negatively impact the developing brain (Jaques, 2014).
Some women report using marijuana to treat severe nausea associated with their pregnancy (Roberson et al., 2014; Westfall et al., 2006); however, there is no research confirming that this is a safe practice, and it is generally not recommended. Women considering using medical marijuana while pregnant should not do so without checking with their health care providers. Animal studies have shown that moderate concentrations of delta-9-tetrahydrocannabinol (or THC, the main psychoactive ingredient in marijuana), when administered to mothers while pregnant or nursing, could have long-lasting effects on the child, including increasing stress responsivity and abnormal patterns of social interactions (Trezza et al., 2008). Animal studies also show learning deficits in prenatally exposed individuals (Antonelli et al., 2005; Mereu et al., 2003).
Human research has shown that some babies born to women who used marijuana during their pregnancies display altered responses to visual stimuli, increased trembling, and a high-pitched cry (Fried & Makin, 1987), which could indicate problems with neurological development (de Moraes et al., 2008). In school, marijuana-exposed children are more likely to show gaps in problem-solving skills, memory (Richardson et al., 2002), and the ability to remain attentive (Goldschmidt et al., 2000). More research is needed, however, to disentangle marijuana-specific effects from those of other environmental factors that could be associated with a mother’s marijuana use, such as an impoverished home environment or the mother’s use of other drugs (Schempf & Strobino, 2008). Prenatal marijuana exposure is also associated with an increased likelihood of a person using marijuana as a young adult, even when other factors that influence drug use are considered (Sonon et al., 2015). More information on marijuana use during pregnancy can be found in NIDA’s Marijuana Research Report.
Very little is known about marijuana use and breastfeeding. One study suggests that moderate amounts of THC find their way into breast milk when a nursing mother uses marijuana (Perez-Reyes & Wall, 1982). Some evidence shows that exposure to THC through breast milk in the first month of life could result in decreased motor development at 1 year of age (Astley & Little, 1990). There have been no studies to determine if exposure to THC during nursing is linked to effects later in the child’s life. With regular use, THC can accumulate in human breast milk to high concentrations(Perez-Reyes & Wall, 1982). Because a baby’s brain is still forming, THC consumed in breast milk could affect brain development. Given all these uncertainties, nursing mothers are discouraged from using marijuana (Djulus et al., 2005). New mothers using medical marijuana should be vigilant about coordinating care between the doctor recommending their marijuana use and the pediatrician caring for their baby.
Stimulants (Cocaine and Methamphetamine)
Some may recall news items about “crack babies,” a term coined in the 1980s to describe babies born to mothers who smoked cocaine while pregnant. These babies were initially predicted to suffer from severe, irreversible cognitive and behavioral consequences, including reduced intelligence and social skills. These purported effects turned out to be somewhat exaggerated. However, it is not completely known how a pregnant woman’s cocaine use affects her child, since cocaine-using women are more likely to also use other drugs such as alcohol, to have poor nutrition, or to not seek prenatal care. All of these factors can affect a developing fetus, making it difficult to isolate the effects of cocaine (Cain et al., 2013).
Research does show, however, that pregnant women who use cocaine are at higher risk for maternal migraines and seizures, premature membrane rupture, and placental abruption (separation of the placental lining from the uterus) (Wendell, 2013). Pregnancy is accompanied by normal cardiovascular changes, and cocaine abuse exacerbates these changes—sometimes leading to serious problems with high blood pressure (hypertensive crises), spontaneous miscarriage, preterm labor, and difficult delivery (Cain et al., 2013). Babies born to mothers who use cocaine during pregnancy may also have low birth weight and smaller head circumferences, and are shorter in length than babies born to mothers who do not use cocaine. They also show symptoms of irritability, hyperactivity, tremors, high-pitched cry, and excessive sucking at birth (Bauer et al., 2005). These symptoms may be due to the effects of cocaine itself, rather than withdrawal, since cocaine and its metabolites are still present in the baby’s body up to 5 to 7 days after delivery (Chasnoff et al., 1986; Eyler et al., 2001).
Pregnant women who use methamphetamine have a greater risk of preeclampsia (high blood pressure and possible organ damage) (Gorman et al., 2014), premature delivery, and placental abruption. Their babies are more likely to be smaller and to have low birth weight (Smith et al., 2006). In a large, longitudinal study of children prenatally exposed to methamphetamine, exposed children had increased emotional reactivity and anxiety/depression, were more withdrawn, had problems with attention, and showed cognitive problems that could lead to poorer academic outcomes (Diaz et al., 2014; LaGasse et al., 2012).
MDMA (Ecstasy, Molly)
What little research exists on the effects of MDMA use in pregnancy suggests that prenatal MDMA exposure may cause learning, memory (Schaefer et al., 2013), and motor problems in the baby (Singer et al., 2012). More research is needed on this topic.
Heroin
Heroin use during pregnancy can result in neonatal abstinence syndrome (NAS). NAS occurs when heroin passes through the placenta to the fetus during pregnancy, causing the baby to become dependent on opioids. Symptoms include excessive crying, high-pitched cry, irritability, seizures, and gastrointestinal problems, among others(Bandstra et al., 2010). NAS requires hospitalization of the affected infant and possibly treatment with morphine or methadone to relieve symptoms (Hudak et al., 2012); researchers have also studied buprenorphine for this purpose (Kraft et al., 2011). The medication is gradually tapered off until the baby adjusts to being opioid-free.
Medications
Prescription and Over-the-Counter (OTC) Drugs
Pregnancy can be a confusing time for pregnant women facing many choices about legal drugs, like tobacco and alcohol, as well as prescription and over-the-counter (OTC) drugs that may affect their baby. These are difficult issues for researchers to study because scientists cannot give potentially dangerous drugs to pregnant women. Here are some of the known facts about popular medications and pregnancy:
There are more than 6 million pregnancies in the United States every year, and pregnant women take an average of three to five prescription drugs while pregnant. The U.S. Food and Drug Administration recently issued new rules on drug labeling to provide clearer instructions for pregnant and nursing women, including a summary of the risks of use during pregnancy and breastfeeding, a discussion of the data supporting the summary, and other information to help prescribers make safe decisions (FDA issues final rule, 2014).
Even so, we know little about the effects of taking most medications during pregnancy. This is because pregnant women are often not included in studies to determine safety of new medications before they come on the market(Pregnancy: Medications and Pregnancy, 2014). A recent study shows that use of short-acting prescription opioids such as oxycodone during pregnancy, especially when combined with tobacco and/or certain antidepressant medications, is associated with an increased likelihood of neonatal abstinence syndrome (NAS) in the infant (Patrick et al., 2015).
Although some prescription and OTC medications are safe to take during pregnancy, a pregnant woman should tell her doctor about all prescription medications, OTC cold and pain medicines, and herbal or dietary supplements she is taking or planning to take. This will allow her doctor to weigh the risks and benefits of a medication during pregnancy. In some cases, the doctor may recommend the continued use of specific medications, even though they could have some impact on the fetus. Suddenly stopping the use of a medication may be more risky for both the mother and baby than continuing to use the medication while under a doctor’s care (Pregnancy: Medications and Pregnancy, 2014). This could also include medications to treat substance use disorders—something that is discussed in further detail in the “Sex and Gender Differences in Substance Use Disorder Treatment” section.
Some prescription and OTC medications are generally compatible with breastfeeding, and the American Academy of Pediatrics maintains a list of such substances. Others, such as some anti-anxiety and antidepressant medications, have unknown effects (AAP Committee on Drugs, 2001), so mothers who are using these medications should consult with their doctor before breastfeeding. Nursing mothers should contact their infant’s health care provider if their infants show any of these reactions to the breast milk: diarrhea, excessive crying, vomiting, skin rashes, loss of appetite, or sleepiness(Ages & Stages, 2014).
Other Substances
Alcohol
Alcohol use while pregnant can result in Fetal Alcohol Spectrum Disorders (FASD), a general term that includes Fetal Alcohol Syndrome, partial Fetal Alcohol Syndrome, alcohol-related disorders of brain development, and alcohol-related birth defects. These effects can last throughout life, causing difficulties with motor coordination, emotional control, schoolwork, socialization, and holding a job. More information can be found on the NIAAA Fetal Alcohol Exposure webpage.
There is currently little research into how a nursing mother’s alcohol use might affect her breastfed baby. What science suggests is that, contrary to folklore, alcohol does not increase a nursing mother’s milk production, and it may disrupt the breastfed child’s sleep cycle (Mennella, n.d.). TheAmerican Academy of Pediatrics recommends that alcohol drinking should be minimized during the months a woman nurses and daily intake limited to no more than 2 ounces of liquor, 8 ounces of wine, or two average beers for a 130-pound woman. In this case, nursing should take place at least 2 hours after drinking to allow the alcohol to be reduced or eliminated from the mother’s body and milk. This will minimize the amount of alcohol passed to the baby(AAP, 2012).
More information can be found in the NIAAA publicationAlcohol’s Effect on Lactation.
Nicotine (Tobacco Products and e-Cigarettes)
Almost 16 percent of pregnant women in the United States have smoked in the past month (SAMHSA, 2014). Carbon monoxide and nicotine from tobacco smoke may interfere with the oxygen supply to the fetus. Nicotine also readily crosses the placenta, and concentrations of this drug in the blood of the fetus can be as much as 15 percent higher than in the mother (Wickström, 2007). Smoking during pregnancy increases the risk for certain birth defects, premature birth, miscarriage, and low birth weight (Reproductive Health, 2014) and is estimated to have caused 1,015 infant deaths annually from 2005 through 2009 (CDC, 2014). Newborns of smoking mothers also show signs of stress and drug withdrawal consistent with what has been reported in infants exposed to other drugs. In some cases, smoking during pregnancy may be associated with sudden infant death syndrome (SIDS), as well as learning and behavioral problems and an increased risk of obesity in children. In addition, smoking more than one pack a day during pregnancy nearly doubles the risk that the affected child will become addicted to tobacco if that child starts smoking (Rydell et al., 2014). Even a mother’s secondhand exposure to cigarette smoke can cause problems; such exposure is associated with premature birth and low birth weight, for example (Khader et al., 2011). The U.S. Department of Health and Human Services providesresources specifically designed to help pregnant women quit smoking.
Recent research provides strong support that nicotine is a gateway drug, making the brain more sensitive to the effects of other drugs such as cocaine (NIH study examines nicotine, 2011). This shows that pregnant women who use nicotine may be affecting their baby’s brain in ways they may not anticipate. Because e-cigarettes typically also contain nicotine, those products may also pose a risk to the baby’s health. More research is needed.
Similar to pregnant women, nursing mothers are also advised against using tobacco. New mothers who smoke should be aware that nicotine is passed through breast milk(Mennella et al., 2007), so tobacco use can impact the infant’s brain and body development—even if the mother never smokes near the baby. There is also evidence that the milk of mothers who smoke smells and may taste like cigarettes. It is unclear whether this will make it more likely that exposed children may find tobacco flavors/smells more appealing later in life (Mennella & Beauchamp, 1998).
Secondhand Smoke
Newborns exposed to secondhand smoke are at greater risk for SIDS, respiratory illnesses (asthma, respiratory infections, and bronchitis), ear infections (Smoking & Tobacco Use, 2015), cavities (Aligne et al., 2003), and increased medical visits and hospitalizations (Leung et al., 2004). If a woman smokes and is planning a pregnancy, the ideal time to seek smoking cessation help is before she becomes pregnant.

